Type 1 diabetes patients in Alberta are now eligible for a therapy program that allows them to switch from daily injections to free insulin pumps.
The provincial government announced funding for the program on March 7.
While organizations such as the Canadian Diabetes Association welcome the decision, some researchers question whether the pumps are the right choice for everyone.
Jeffrey Johnson, scientific director for obesity, diabetes and nutrition and professor at the school of public health at the University of Alberta, said the pump only benefits a small number of people whose lifestyle does not allow day-to-day injections.
“The benefit of a pump is that it replaces multiple daily insulin injections but those people still have to pay a lot of attention to their insulin pump and their regular testing of their blood sugars,” he said.
“Proper use requires considerable attention and self care.”
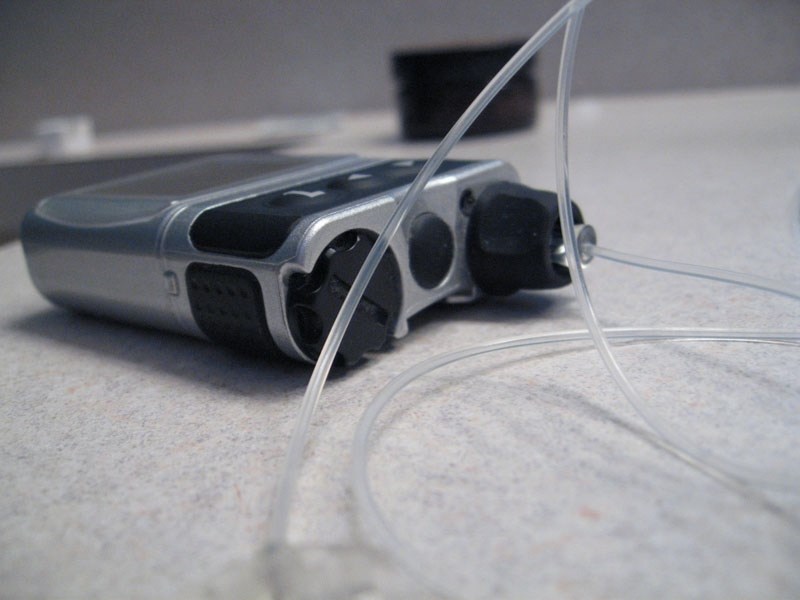
Insulin pumps are about the size of a pager. They are portable and patients can program them to deliver insulin through a plastic tube connected to a small needle under their skin.
According to the Canadian Diabetes Association, switching from daily insulin injections to an insulin pump can offer better control of blood sugar levels and increase the quality of life for those living with type 1 diabetes.
Johnson said some associations claim the pump aids patients to avoid long-term complications related to diabetes, such as kidney failure, and damage to the eyes or nerves. Avoiding these could save the health-care system money.
He said there is no evidence to support these claims, or to support the huge cost of the pumps. They cost about $7,000 to buy and about $2,000 dollars worth of supplies a year. They must also be replaced every four to five years.
“I recognize there are some people, their lifestyle is better managed with the pump,” he said.
“But the evidence doesn’t support the claims being made and sometimes they are made as advocacy efforts to convince the government.”
Instead, he said diabetes-care teams with nurses, dietitians and pharmacists would benefit the public in the long run as they can discuss and follow up with patients for treatments and medications.
The Canadian Diabetes Association expects diabetes numbers in Alberta to rise from 245,000 people in 2012, to 544,000 in 2032.
Those living with type 1 diabetes are estimated at 13,800, with numbers expected to reach 24,400 by 2032.
Johnson said in a community such as St. Albert, about 1,400 people live with type 1 diabetes. About 400 or 500 of these people may benefit from having the pump.
Those who apply for the pump need training to use it properly, he added. If the pump breaks down or the line gets blocked, people can experience serious health risks.
They consistently need to check the amount of insulin in the pump, and carefully measure how much they need to inject.
His main concern is that people take too much or not enough insulin, which can lead to a coma or seizure.
“A lot of people have the mistaken perception that it’s a plug-and-play and in fact it’s probably more work than regular daily injections,” he said.
“It’s a good thing that the government is considering a program for insulin pumps but it’s also a good thing that the government is taking a prudent approach and develops a policy to evaluate the long term benefit.”